profile/833629462068-66AD-4E14-8E2E-2E355A35CE2B.jpeg
Scientist
Your Destiny Is In Your DNA
~1.0 mins read
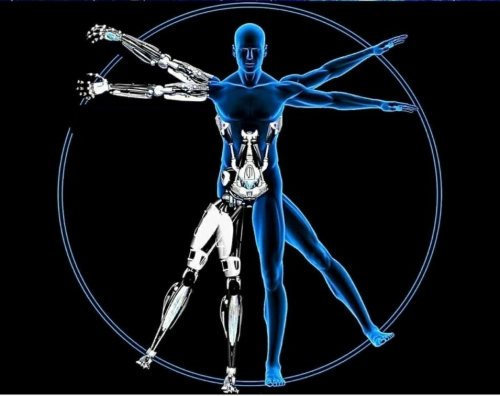
The future is full of amazing opportunities, beyond anything we can imagine today. DNA preservation, and the possibilities of human cloning, offer you a unique chance to be part of that future.
There are many reasons why people consider cloning. Some are suffering from debilitating diseases that will inevitably be cured in the future. Others are nearing the end of their natural life and want to create a new version of themselves in the hope of extending the experience. Some even see their future on another world, as colony ships transport DNA to new planets to seed new life.
Whatever the reason for your interest, Cloning technology is here to make sure your DNA is still around when technology, politics and ethics come together to make human cloning possible.
The science already exists, so it is only a matter of time before human cloning happens.
There are many reasons why people consider cloning. Some are suffering from debilitating diseases that will inevitably be cured in the future. Others are nearing the end of their natural life and want to create a new version of themselves in the hope of extending the experience. Some even see their future on another world, as colony ships transport DNA to new planets to seed new life.
Whatever the reason for your interest, Cloning technology is here to make sure your DNA is still around when technology, politics and ethics come together to make human cloning possible.
The science already exists, so it is only a matter of time before human cloning happens.
What is your take on Cloning?
profile/833629462068-66AD-4E14-8E2E-2E355A35CE2B.jpeg
Scientist

Must Read: Highlights Of The True Buddha's Life
~3.2 mins read
He said, “I am not God. I am not a Deva. Nor am I a Human… I am the Awakened one, who has seen the Truth of the world.”
He did a meticulous analysis of his mind in such a way that he was able to count all the atoms in his body.
He said, “Nothing in this world is solid.” The modern meaning of which is that everything is made up of tiny particles and these particles are repeatedly broken down and reformed. He was well aware of the quantum level of existence.
He was famous for another reason that he taught people of all languages in their own language whoever met him. Although he chose the Pali language of the common people during discoursing in the assembly.
No animal would ever harm him while meditating in the deep forest. It is believed that the animals were attracted to him, they looked at him calmly because of the power of his Metta (amity, benevolence).
He gave the theory of rebirth. He observed himself spontaneously and said that he had become the ‘Buddha’ in this birth because of the good deeds of all previous births.
He said that the ultimate goal of life is Nibbana, which means liberation from the cycle of life and death.
A serial killer like Angulimala who killed 999 people, city prostitute like Amrapali, controversialist like Saccaka and Upali who challenged Buddha, all of them were initiated into his religion and became Arhants!
From a very young age he would never make jokes, never gossiped, never made fun, but always had a glimpse of smile on his face that fascinated everyone.
One day, while he was going for alms, a little boy picked up a bowl of dust in front of Buddha. Buddha smiled softly and took the alms bowl forward. When Ananda asked the reason for Buddha's laughter, Buddha said, “This boy will reborn in the city of Pataliputta two and half years after my parinibbana (death) and will be the chakkavatti (wheel turning) emperor and will make history by building 84,000 metal temples and shrines for the benefit of Buddhist rule.” He was no one else, the emperor Great Ashoka!
He had a very good look, blue eyes, broad shoulders, long ears, mild crimped hair and was full of benevolence and mercy. It is said that a bright halo would come out of his fair body (the complexion appeared clearer and brighter on two occasions, before the moment of enlightenment and before the moment of parinibbana).
He was born (623 BCE), enlightened (588 BCE) and attained parinibbana (543 BCE) on the same day. This day is the full moon day of Vesakha (May).
Among Buddha's many disciples, Ananda stood out for having the best memory. Most of the texts of the early Buddhist Sutta Piṭaka are attributed to his pure recollection of Buddha's teachings during the First Buddhist Council.
Today his religion is considered the most scientific religion and there are some variations of it, it happened over time.
Buddha gave such knowledge of mind and body as it really is, not in the way of any religious belief!
The monk has always fasted in his life and taught by traveling long distances on foot till his parinibbana.
After attaining enlightenment, he reunited with his family and guided his father, mother, wife and son to Nibbana. Happy family!
This great scientist was born more than 2600 years ago and his non-violence, Metta teaching and meditation techniques are still practiced which is appreciated all over the world.
The most fascinating thing about Buddha is that we can see him as a Human like us!
A man with a beautiful mind. He is not God, nor a god, nor a prophet. He is perfect just as a human being. Lived and died like human beings. There is no promise of heaven in his religion. No threat of hell. No need to pray. No compulsory to follow him. No mandatory rituals.
Following his teachings makes one a better person. The Dhamma is not harmed if one does not follow it. He/she will just miss the opportunity to be a better human.
Source: Supayan Chakma Gautam on Quora
Advertisement
Link socials
Matches
Loading...
