
Doctors worldwide are overwhelmed with the number of patients reporting infected toes. They find it highly unlikely, as it usually happens during extremely cold winters. However, it’s a sign that can’t be ignored. We got in touch with Dr Swati Mohan, Dermatologist at Fortis, Faridabad to tell us all about the newfound symptom.
What is COVID toe?
 Image Credit: istock
Image Credit: istockCOVID toe patients have good immunity

The good news is that patients with these lesions are doing well and seem to have good immunity, so they shouldn't panic. Dr Swati suggests, “These patients should not rush to emergency and risk exposing themselves and others to the virus. Instead, they should take rest and if there is itching, they should apply local hydrocortisone. If there is pain, then they can take Aspirin. Under such circumstances, social distancing is a must.â€
 Image Credit: istock
Image Credit: istock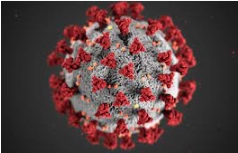
Advertisement
Link socials
Matches
